Breast Reconstruction with Implants
Implant-Based Breast Reconstruction
Breast reconstruction is a significant aspect of the journey for many women who have undergone mastectomy due to breast cancer or other medical reasons. Among the various options available, implant-based breast reconstruction is a popular and effective choice. In fact, over 75% of breast reconstructions performed worldwide are with implants. This webpage aims to provide detailed information on implant-based breast reconstruction, covering indications, risks, recovery, and potential complications.
Introduction
Implant-based breast reconstruction involves the use of implants to recreate the breast mound. This method is suitable for many women, but it is essential to understand the indications, potential risks, recovery process, and potential complications associated with this procedure.
Breast Implants – The Basics
A breast implant is a device that is designed to reconstruct a breast mound
There are a few variables in selecting a breast implant
- Shape – Breast implants can be either anatomical (“tear drop”), where they are roughly shaped like a normal breast, or round. A/Prof Marucci prefers to use anatomical implants in breast reconstruction (and round implants for cosmetic augmentation)
- Implant Texture – The outside surface of a breast implant can either be smooth or textured. Texturing was originally performed to decrease capsule formation. However, textured surfaces have been associated with the very rare occurrence of Anaplastic Large Cell Lymphoma (ALCL). ALCL may present with a fluid accumulation around an implant 5 – 10 years after the implants were placed. All anatomical implants are textured.
- Volume – Implants come in various volumes. There are only a finite range of implant volumes produced, and it is not always possible to find an implant shape and volume that will exactly match the breast that has been removed.
- Implant Fill – All implants used in Australia are filled with cohesive silicone gel. This has the consistency of Turkish Delight. Saline implants aren’t used in Australia (and are terrible implants, so we aren’t missing anything there).
- Tissue Expander Vs Implant– A tissue expander is a special kind of breast implant. It is like an empty implant into which fluid can be injected in order to increase its volume. It is used in situations where there is not enough loose skin for the correct size implant to be placed. Once the tissue expander is in place, extra fluid can be added to the expander in the weeks and months after the surgery by placing a needle through the chest skin into the port of the expander. This expander port can be accessed whenever necessary to slowly increase the volume of fluid within the expander, which has the effect of stretching the surrounding skin. Once the breast mound has reached the desired volume as a result of the tissue expansion, the breast tissue expander can be replaced with a definitive breast implant in a second surgical procedure. Another potential sequence involving a tissue expander is where a patient desires a flap reconstruction, but needs radiotherapy after the mastectomy. In these cases, the tissue expander can be used as a “placeholder” to preserve the skin of the chest wall and give the patient a breast mound while they go through radiotherapy. The expander can later be removed and replaced with a free flap is the patient so desires – this is called a “delayed immediate” reconstruction.
Potential Stages in Implant Based Breast Reconstruction
Implant based breast reconstruction can be performed in either one or two stages. The decision will depend on many factors, including the likelihood of post operative radiotherapy, the quality of the skin and soft tissue on the breast and whether the patient ultimately wants a tissue reconstruction.
Single-Stage Implant-Based Breast Reconstruction (Direct to Implant):
Single-stage breast reconstruction, also known as direct-to-implant (DTI) reconstruction, involves placing the implant immediately after the mastectomy in a single surgery. This streamlined approach offers several compelling advantages:
- Immediate Results:
One of the most significant benefits of a single-stage reconstruction is the immediate restoration of breast volume. Patients wake up from surgery with a reconstructed breast, minimizing the emotional impact of losing breast tissue during the mastectomy. - Reduced Recovery Time:
Since the entire reconstruction process occurs in a single surgery, patients often experience a shorter overall recovery time compared to multi-stage approaches. This can be particularly appealing for those seeking a quicker return to their normal activities. - Minimized Disruption:
Single-stage reconstruction involves fewer surgeries, leading to less disruption to daily life. This can be advantageous for patients with busy schedules or those looking to streamline their recovery process. “One and its done!”. - Can Proceed with Adjuvant Treatments
As the breast reconstruction has now been completed following DTI, the patient can proceed with adjuvant treatments, such as radiotherapy, knowing that (hopefully) their visits to the operating theatre are behind them. However, adjuvant radiotherapy may impact the cosmetic outcome of the reconstruction. Some patients may require further surgery, or even replacement of the implant should complications occur.
Despite these advantages, there are some considerations and potential disadvantages associated with single-stage implant-based reconstruction:
- Limitations in Adjustability:
The immediate placement of the implant may limit the surgeon’s ability to fine-tune the final result. Adjusting the size or shape of the reconstructed breast may be more challenging compared to a two-stage approach. - Risk of Complications:
While complications are possible with any surgical procedure, the risk may be slightly higher in single-stage reconstruction due to the complexity of combining mastectomy and implant placement in a single session. This is still a subject of ongoing research.
Two-Stage Implant-Based Breast Reconstruction:
Two-stage implant-based breast reconstruction is a phased approach that provides greater flexibility and precision. Here are the key advantages of this method:
- Tissue Expansion:
In the first stage, a tissue expander is placed beneath the chest muscle. This device gradually expands the skin and tissue to create a suitable pocket for the final implant. This allows for a more customized and adjustable outcome. - Size Adjustability:
Two-stage reconstruction allows for size adjustments during the expansion process. This flexibility is particularly beneficial for patients who want more control over the final aesthetic result or those uncertain about the desired size. - Improved Aesthetics:
Surgeons can modify the breast pocket and refine the shape during the second stage, enhancing the overall result.
However, there are potential downsides to consider with two-stage reconstruction:
- Extended Timeline:
The overall process of two-stage reconstruction takes longer than the single-stage approach. Patients undergo multiple surgeries and require time for tissue expansion before the final implant is placed, extending the reconstruction timeline. - Additional Recovery Periods:
Each stage of the reconstruction process involves its own recovery period, which may be a consideration for those seeking a more expedited recovery. - Additional Surgery with Additional Risks:
All surgical procedures involve risk. Having additional procedures, by definition, increases that risk.
Practical Details of Implant Based Breast Reconstruction
Every surgeon has a slightly different technique for implant based breast reconstruction. Here is a rough outline of A/Prof Marucci’s techniques and recommendations.
Before the Surgery
- Buy two of the bras shown to you by A/Prof Marucci that have no underwire and do up in the front. Be holding one of the bras in your hand as you go in for the operation. Don’t pack it in your bag
- You will be told a few days before the surgery when to be at the hospital and when to stop eating and drinking
The Surgery Itself
- On the day of the surgery you will be checked into the hospital. You will meet the anaesthetist
- A/Prof Marucci will draw the surgical plan on you before you go into the operating theatre. Your bra will be collected at this point and you will go into the operating theatre for the procedure
- The surgery is performed under general anaesthesia – you will be completely asleep. Antibiotics will be started
- The first part of the operation involves the breast surgeon removing the breast tissue. This is sent off to the lab for analysis
- A/Prof Marucci will then perform the breast reconstruction using an implant. In some cases, a silicone implant of an appropriate shape and size can be put straight into the wound. Where this is not possible, a different type of implant called an “expander” is partially filled with saline and put into the wound instead.
- A/Prof Marucci prefers to put the implant in front of the chest wall muscle whenever possible, as this has been shown to give a better cosmetic result, decrease pain, and prevent the implant moving when the chest wall muscles are flexed
- Drains are always used. They are hollow tubes about as thick as your little finger that drain fluid into a small cannister. You will be shown how to measure the drain output after the surgery
- After the implant has been carefully placed and the wound closed with dissolving sutures, A/Prof Marucci will put local anaesthetic and further antibiotics around the implant via the drain
- A clear see-through plastic dressing is placed on the wound so the blood flow to the area can be easily assessed after the surgery. You are then placed into the bra and you go into recovery to wake up fully
After the surgery
- Once you have woken up, you can get out of bed and walk around. Some patients stay in hospital for one or two nights
- The local anaesthetic will last for many hours. You will be given a script for stronger painkillers to be used when the local anaesthetic wears off
- The drains are important, but a hassle. You can’t shower between your neck and your navel until the drains have been removed. The drains stay in until they are draining less than 30 ml per day for 2 days in a row. Drains can be in anywhere from 1 – 3 weeks
- Wear one of the soft non underwire bras day and night until the drains are removed
- One of the most serious potential early complications is infection. Everything is done to prevent an infection. You will be given one week of tablet antibiotics after the surgery and you will be reviewed weekly until the drains come out. If there is spreading redness / increasing pain / swelling / signs of infection, please let the rooms or A/Prof Marucci know ASAP
- It is common for there to be bruising of the breasts. Initially the skin is purple, then it goes green/yellow. It is very common for their to be rippling of the skin, but this tends to settle down after a period of months.
- Most patients are driving within a week or so of their surgery
- It is normal to need a “nanna-nap” in the afternoon for a week or so after the surgery and most patients can return to light duties work after the drains come out
- No swimming and no exercise until a week or two after the drains come out. Nothing “for” exercise (you can walk – but not for exercise)
- It takes a few months for everything to settle down after surgery. The key thing is: if any problems or any concerns, contact A/Prof Marucci via the rooms
- If a silicone implant was placed at the time of surgery, that means that the reconstruction has been completed
- If a tissue expander was placed, the reconstruction is not yet complete. Starting from a few weeks after the surgery further fluid will be placed into the expander by putting a needle through the skin. Once an appropriate volume has been achieved (and, if appropriate, the effects of post operative radiotherapy have settled down) the expander will need to be replaced with something to complete the reconstruction. Most commonly, the expander is exchanged for a silicone implant. This is a much smaller procedure than the original mastectomy and expander placement. Sometimes, the expander is replaced with a patient’s own tissue (a “flap” usually taken from the abdomen)
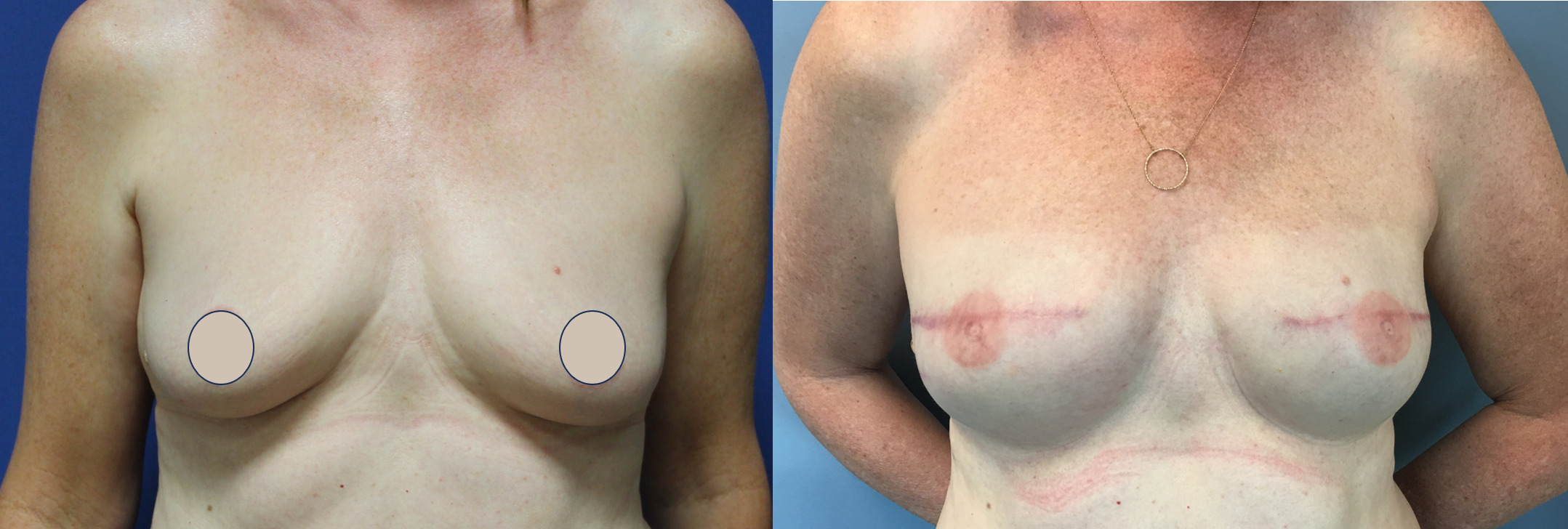
Before and After Photos
This patient had bilateral mastectomies and underwent immediate implant-based breast reconstruction by A/Prof Damian Marucci. Nipple tatoos were later performed.
Risks Associated with Implant-Based Breast Reconstruction
- Infection:
– Infections are a potential risk after any surgery, but especially with implant based breast reconstruction. There is a risk of significant infection requiring admission to hospital, intravenous antibiotics, potentially surgery to replace an infected device, and, occasionally, the need to remove the implant completely to allow the infection to settle down. The incidence of serious infections, even in the most experienced of hands, is in the order of 10% of cases. Antibiotics are typically prescribed to minimize this risk. - Implant Rupture or Leakage:
– Implants may rupture or leak over time, necessitating additional surgery to replace or remove the implant. - Capsular Contracture:
– The body naturally forms a scar tissue capsule around the implant. In some cases, this capsule may “contract” or become fibrotic, causing the breast to feel firm or distorted. There are a number of different levels of “capsular contracture”. Milder grades of capsular contracture may result in implant rippling or visibility. More severe grades of capsular contracture may result distortion of the shape of the breast and even cause pain.Revision surgery may be required to address severe cases of capsular contracture. - Changes in Breast Sensation:
– Mastectomy surgery involves dividing most if not all of the nerves that supple the breast skin with sensation. Numbness or changes in breast sensation are common after surgery. While sensation may gradually improve, it may not fully return to pre-surgery levels. - Implant movement or malposition:
– Breast implantsdon’t behave like normal breast tissue. Sometimes implants can move with chest muscle movement (although this is more likely if the implants are placed underneath the chest muscles, something which A/Prof Marucci rarely does). Implants can also move – they may migrate towards the arms pits, or sometimes they can sit too high. - Anaplastic Large Cell Lymphoma:
– There is a rare form of blood cancer (lymphoma) that can develop in the capsule around a breast implant. It is called Anaplastic Large Cell Lymphoma (ALCL). A lot of research is still going on into ALCL and there is still many things about the condition that we don’t know. It appears to be related to bugs that get onto the texturing of the implant when they are put in, causing an inflammatory reaction that can (in some patients) develop into a lymphoma. ALCL usually presents with a fluid accumulation around the implant more than 5 years after the implants were placed. The diagnosis is made via a biopsy. Treatment usually involves initially removing the implant and the diseased capsule – although a later breast reconstruction can almost always be performed.
Recovery Process after Implant-Based Breast Reconstruction
- Hospital Stay:
– Patients have a reconstruction of one breast are usually able to go home after one or two nights in hospital. In cases where both breasts are being reconstructed, most patients stay in for 2 nights. Antibiotics are initially given through the IV drip but patients usually go home with one week of tablet antibiotics. Patients will be shown how to empty their drains and measure the output while they are in hospital. - Activity Restrictions:
– Patients have to wear a bra with no underwire that does up in the front day and night until the drains come out.
– Patients are asked to measure how much fluid is coming out of their breast drains. When the output is less than 30mls in 24 hours for 2 days in a row, that drain can then come out
– Patients are to keep the breast area and drains completely dry. The best way to think of this is that everything between the neck and navel needs to stay dry.
– No exercise until A/Prof Marucci gives the OK. Even light exercise. And nothing “for” exercise – so you can walk, but not “for exercise”.
– Once the drains are out, patients can shower normally - Pain Management:
– Pain and discomfort are normal after surgery, and pain medications will be prescribed. - Follow-Up Appointments:
– A/Prof Marucci usually sees all his implant-based breast reconstruction patients until the week after the drains come out. Patients are usually seen again a few months after their surgery. Patients with implants need to be followed up every year for as long as they have their implants. - Emotional Support:
– Breast reconstruction is not only a physical but also an emotional journey. A/Prof Marucci works closely with the Breast Care Nurses working at St George Public and Private Hospitals.
Complications of Implant-Based Breast Reconstruction
- Delayed Wound Healing:
Some patients may experience delayed wound healing of the mastectomy woundx, especially if they have other health issues that affect the healing process. Patients must not smoke within 4 weeks of surgery. Patients with a history of radiotherapy to the chest wall are at a particularly high risk of wound healing problems. - Symmetry Issues:
Achieving perfect symmetry between a reconstructed breast and a natural breast is not possible. Additional surgeries may be needed to improve symmetry, but there will always be differences in shape, feel and behaviour - Implant Malposition:
Implants may shift or settle unevenly over time, requiring revision surgery to correct the position. - Unsatisfactory Aesthetic Outcome:
While efforts are made to achieve a natural appearance, some patients may be dissatisfied with the aesthetic outcome. Revision surgeries may be considered to address these concerns. There may be the option of replacing the implant with a patient’s own tissue (autologous reconstruction). Autologous reconstructions are considered by many to be the “gold standard” type of reconstruction, although the associated surgery is more extensive than implant-based breast reconstruction. - Psychological Impact:
A mastectomy procedure commonly results in psychological challenges related to body image and self-esteem. Counselling and support groups can be valuable resources in addressing these concerns. A/Prof Marucci works closely with the breast care nurses at St George Public and Private Hospitals to provide holistic support to patients undergoing reconstruction.
Conclusion
Implant-based breast reconstruction is a valuable option for women seeking to restore their breasts after mastectomy. Understanding the indications, risks, recovery process, and potential complications is crucial for making informed decisions. It is essential for patients to work closely with their healthcare team to ensure the best possible outcome and to receive the necessary support throughout the reconstruction journey. By providing comprehensive information, this guide aims to empower women to make informed choices and navigate the challenges of implant-based breast reconstruction with confidence.
It is also important to choose an experienced surgeon to perform your breast reconstruction. Look for a surgeon who is a Fellow of the Royal Australasian College of Surgeons (FRACS) and is a member of the Australian Society of Plastic Surgeons (ASPS) as well as the Australasian Society of Aesthetic Plastic Surgeons (ASAPS). A/Prof Marucci has a FRACS in Plastic and Reconstructive Surgery. He is on the Education Committee of ASPS and is on the Board of ASAPS. A/Prof Marucci is registered a specialist in Plastic and Reconstructive surgery with AHPRA.