Skin Graft Surgery for Skin Cancer
Skin grafts are surgical procedures used to reconstruct skin loss after excision of a skin cancer, when there isn’t enough local tissue to simply close the wound with stiches. It involves the transplantation of skin from one part of the body (donor site) to another part of the body (recipient site). Skin grafts are typically used to treat large or complex wounds or areas of skin loss. In addition to skin cancer treatment, skin grafts may also be used to reconstruct wounds due to trauma or burns.
Understanding Split-Thickness Skin Grafts
In a split-thickness skin graft, the surgeon removes a thin layer of skin from the donor site, usually from the leg or upper inner arm.This layer includes the epidermis, the outer layer of skin, and part of the dermis, the middle layer of skin. The donor site is then allowed to heal on its own over a couple of weeks.
Benefits of Split-Thickness Skin Grafts:
- Rapid healing: Split-thickness grafts heal relatively quickly, as the remaining dermis can regenerate new skin cells.
- Less donor site trauma: Removing a thin layer of skin creates less discomfort and scarring at the donor site.
- Large coverage: Split-thickness grafts can cover large areas of the body.
Complications of Split-Thickness Skin Grafts:
- Graft failure: The graft may not take hold and may require a second procedure.
- Contraction: The graft may shrink and tighten, causing distortion or impaired function.
- Scarring: The donor site may develop a noticeable scar.
- Loss of sensation: The grafted area may experience reduced or altered sensation.
- Contour and colour changes: Split skin grafts tend to be much thicker than the skin that has been removed. This means that there is often a depression where the skin graft has been placed. Skin grafts often end up a different colour to the surrounding skin, causing a permanent colour mismatch.
Split Skin Grafts to the Legs
Skin cancers on the legs are very common. There is not a lot of loose skin on the lower legs in particular, so skin grafts are commonly performed following skin cancer excision. Here is an outline of what is involved with split skin grafting for lower leg skin cancers:
Before the Surgery
- Stay on all your regular medications including aspirin (Cartia), warfarin (Coumadin) and clopidogrel (Plavix). The ONLY exception is that if you are on blood thinners like Xarelto, Pradaxa or Eliquis – please don’t take the ONE dose BEFORE the surgery, and then go back onto your usual dosage straight after the surgery
- If your surgery is being performed completely under local anaesthetic, you will be given a script for tablet antibiotics which you start taking ON THE DAY OF THE SURGERY. Take ONE tablet before you come in for the surgery. When you go home, you will take one tablet four times a day (breakfast, lunch and dinner and before you go to bed) for FIVE days
The Surgery Itself
- You will be taken into the operating theatre and A/Prof Marucci will draw on you to plan the surgery
- This type of surgery can be performed under “sedation” – where you are made to go to sleep by drugs the anaesthetist puts into your veins, and then local anaesthetic is injected around the area of surgery in the few minutes that you are asleep. It can also be performed under local anaesthesia, where you are fully awake. Either way, local anaesthetic is injected to make the area numb. After that, you will feel some pushing and pulling but you shouldn’t feel anything sharp. If you do, let A/Prof Marucci know and he can put in some more local anaesthetic
- The surgery is performed on two parts of the body: the part where the cancer is being removed, and the part where the “split skin graft” is being taken from
- The most common areas where the skin graft is taken from is the outside or inside of the calf below the knee. After the skin graft has been taken (or “harvested”), a raw area of skin is left at this “donor site”. If the area is small, A/Prof Marucci will dress the donor site with a clear plastic dressing called Tegaderm, which has some holes in it so fluid doesn’t accumulate. The Tegaderm will stay on the wound for a few weeks until the underlying skin has healed back to normal
- The skin graft is usually sutured with dissolving stitches to the edges of the wound left following removal of the cancer
- On top of the skin graft, dressings containing Vaseline, gauze and foam are also stitched or stapled to the edges of the wound. These dressings hold the skin graft in place. The leg is usually wrapped up in many layers from the toes to the knee
After the surgery
- The local anaesthetic will last for a few hours. When it wears off you might need some Panadol, but you shouldn’t need anything stronger than that
- You need to keep the dressings on the leg completely clean, dry and intact. Because all the wounds are below the knee, if you can safely put your leg in a plastic bag and sit on a plastic chair in your shower you will be able to shower every day. The only thing to remember is:the bandages on the leg are to be kept clean, dry and intact until removed by a doctor or nurse
- You need to rest with your leg up as much as possible after the surgery. Either you are lying down with your leg up, sitting down with your leg up, or walking between sitting/lying down with your leg up. That is it. You are taking it easy at home
- The skin graft will usually be inspected 5 – 7 days after the surgery. It will then be wrapped up again from the toes to the knee
- The plastic dressing (Tegaderm) over the donor site (the area where the skin graft came from) stays intact for a few weeks
- The skin graft itself needs to be dressed regularly. There are two ways the leg graft can be dressed – and it will depend on your discussions with A/Prof Marucci as to which one occurs:
- Community Nurse Dressings:
We can arrange for a community nurse to come to your house to do the dressings every Monday, Wednesday and Friday. You will continue to see A/Prof Marucci every week or two until the skin graft has healed (usually 4 – 6 weeks). You can shower with your leg in a plastic bag, but you need to wait around at home until the community nurse arrives on the designated days - You do your own dressings:
For motivated patients with small skin grafts, they can shower every day straight over the wounds (give the graft a gentle clean with your finger). Leave the plastic sheet of Tegaderm on the donor site alone. Pat the graft wound dry after the shower, then butter Vaseline onto a square of gauze, apply the gauze to the skin graft and then put the leg in a stocking (Tubigrip) supplied by A/Prof Marucci. You will continue to see A/Prof Marucci every week or two until the skin graft has healed (usually 4 – 6 weeks).
- Community Nurse Dressings:
Understanding Full-Thickness Skin Grafts
In a full-thickness skin graft, the surgeon removes the entire thickness of skin from the donor site, including both the epidermis and dermis. This type of graft is typically used for smaller defects or cosmetically sensitive areas, such as the face.
Benefits of Full-Thickness Skin Grafts:
- Natural appearance: Full-thickness grafts provide a more natural appearance and texture to the skin, although some colour mismatch may still occur
- Reduced risk of contraction: The graft is less likely to shrink or tighten when compared with a split skin graft, preserving normal function.
- Preserved sensation: The grafted area is more likely to regain sensation after surgery
Complications of Full-Thickness Skin Grafts:
- Donor site closure: The donor site needs to be closed, as it won’t heal on its own like a split skin graft donor site.
- Increased donor site trauma: Removing the entire thickness of skin can cause more discomfort and scarring at the donor site.
- Limited coverage: Full-thickness grafts are typically used for smaller areas due to the increased donor site trauma.
What is involved with a Full Thickness Skin Graft for Skin Cancer Treatment
Before the Surgery
- Stay on all you regular medications including aspirin (Cartia), warfarin (Coumadin) and clopidogrel (Plavix). The ONLY exception is that if you are on blood thinners like Xarelto or Eliquis – please don’t take the ONE dose BEFORE the surgery, and then go back onto your usual dosage straight after the surgery
- You will usually be given a script for tablet antibiotics which you start taking ON THE DAY OF THE SURGERY. Take ONE tablet before you come in for the surgery. When you go home, you will take one tablet four times a day (breakfast, lunch and dinner and before you go to bed) for FIVE days
The Surgery Itself
- You will be taken into the operating room and A/Prof Marucci will draw on you to plan the surgery. This type of surgery is most commonly performed under local anaesthesia, where you are fully awake. Sometimes the surgery is performed under “sedation” – where you are made to go to sleep by drugs the anaesthetist injects and then the local anaesthetic is injected in the few minutes you are out to it. Either way, local anaesthetic is injected to make the area numb. After that, you will feel some pushing and pulling but you shouldn’t feel anything sharp. If you do, let A/Prof Marucci know and he can put in some more local anaesthetic
- The surgery is performed on two parts of the body. The part where the cancer is being removed and the part where the “skin graft” is being taken from. The most common areas where the skin graft is taken from are the collarbone area, or just in front of or just behind the ear. These wounds are usually closed with dissolving sutures
- The skin graft is sutured with dissolving stitches to the edges of the wound left following removal of the cancer. On top of the skin graft dressings containing Vaseline, gauze and foam are also stitched to the edges of the wound. These dressings hold the skin graft in place. You can go home the same day as the surgery
After the surgery
- You need to keep the area where the skin graft is completely dry until the dressings are removed a week later. The area where the skin graft came from (the collarbone area, or just in front of or just behind the ear) can get wet NORMALLY the day after the surgery. Only the area where the skin graft is needs to be kept completely dry
- The skin graft dressing will be removed a week later. Usually after that you can then get the skin graft wet in the shower every day, and apply Vaseline to the skin graft twice a day. Give the skin graft a gentle clean with your finger every time you have a shower to remove any dead layers of skin. You will need to apply the Vaseline for 4 – 6 weeks
- No swimming and no exercise for one week after the surgery. Nothing “for” exercise (you can walk – but not for exercise)
- The local anaesthetic will last for a few hours. When it wears off you might need some Panadol, but you shouldn’t need anything stronger than that
- If there is any bleeding from the wound, put firm pressure on for at least 10 minutes with clean tissues. This should stop 99% of all bleeding. Look at the clock and make sure it is a full 10 minutes. If the bleeding hasn’t stopped after 20 – 30 minutes of pressure, let the rooms or A/Prof Marucci know
- If there is spreading redness / increasing pain / signs of infection, please let the rooms or A/Prof Marucci know
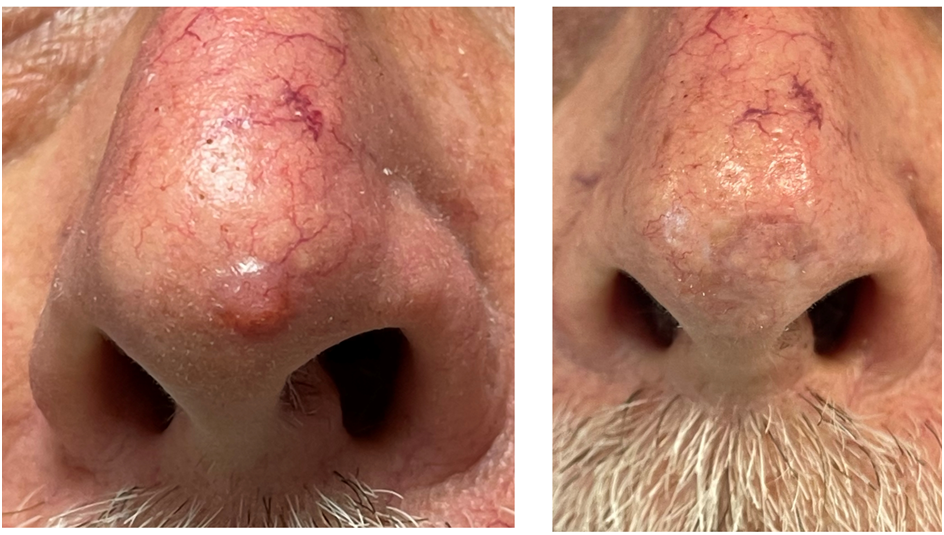
Before and After Photos of Skin Graft Reconstruction
Here is a before and after photo of a patient of A/Prof Damian Marucci who had a full thickness skin graft to the nasal tip following excision of a BCC.
Conclusion
Skin grafting is a versatile and effective surgical procedure that can restore form and function to areas of skin loss. Split-thickness and full-thickness skin grafts are two common techniques with distinct advantages and disadvantages. A/Prof Damian Marucci will work closely with you to determine the most suitable graft type for your specific needs.